Iniziamo questo nuovo anno di newsletter segnalando, fra i più interessanti, quattro articoli, tutti in uscita sul prossimo RAPM.

Teniamo alta l’attenzione sulla sicurezza ed iniziamo con una nostra reply in cui si sottolinea l’importanza del controllo della opening injection pressure assieme alla guida ens ed ecografica durante blocco nervoso periferico.
Costa F, Pascarella G, Del Buono R et Al Opening injection pressure as a part of multimodal monitoring to detect intraneural injections Regional Anesthesia & Pain Medicine Published Online First: 13 January 2022. Opening injection pressure as a part of multimodal monitoring to detect intraneural injections | Regional Anesthesia & Pain Medicine (bmj.com)
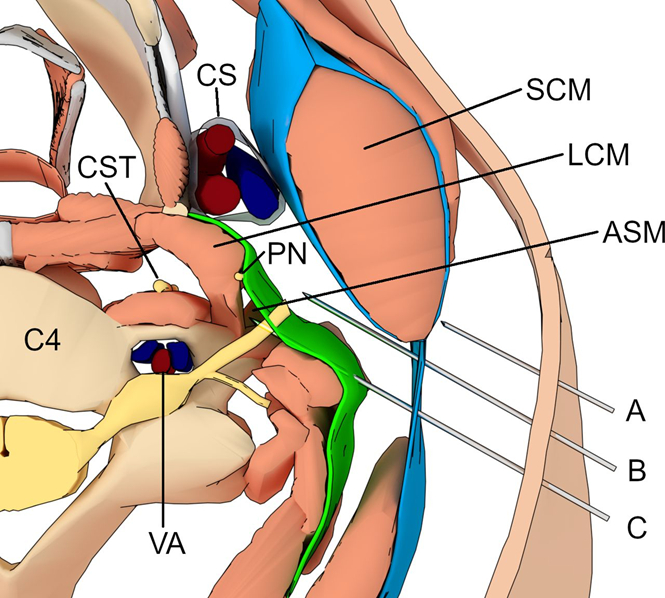
Sempre in tema di sicurezza, torniamo sul blocco del nervo frenico con questi due articoli, il primo ci evidenzia come cambi l’incidenza e l’intensità del blocco del frenico in base alla profondità del blocco del plesso cervicale:
Opperer M, Kaufmann R, Meissnitzer M, et al. Depth of cervical plexus block and phrenic nerve blockade: a randomized trial Reg Anesth Pain Med Epub ahead of print: Depth of cervical plexus block and phrenic nerve blockade: a randomized trial | Regional Anesthesia & Pain Medicine (bmj.com)
Background and objectives Cervical plexus blocks are commonly used to facilitate carotid endarterectomy (CEA) in the awake patient. These blocks can be divided into superficial, intermediate, and deep blocks by their relation to the fasciae of the neck. We hypothesized that the depth of block would have a significant impact on phrenic nerve blockade and consequently hemi-diaphragmatic motion.
Methods We enrolled 45 patients in an observer blinded randomized controlled trial, scheduled for elective, awake CEA. Patients received either deep, intermediate, or superficial cervical plexus blocks, using 20 mL of 0.5% ropivacaine mixed with an MRI contrast agent. Before and after placement of the block, transabdominal ultrasound measurements of diaphragmatic movement were performed. Patients underwent MRI of the neck to evaluate spread of the injectate, as well as lung function measurements. The primary outcome was ipsilateral difference of hemi-diaphragmatic motion during forced inspiration between study groups.
Results Postoperatively, forced inspiration movement of the ipsilateral diaphragm (4.34±1.06, 3.86±1.24, 2.04±1.20 (mean in cm±SD for superficial, intermediate and deep, respectively)) was statistically different between block groups (p<0.001). Differences were also seen during normal inspiration. Lung function, oxygen saturation, complication rates, and patient satisfaction did not differ. MRI studies indicated pronounced permeation across the superficial fascia, but nevertheless easily distinguishable spread of injectate within the targeted compartments.
Conclusions We studied the characteristics and side effects of cervical plexus blocks by depth of injection. Diaphragmatic dysfunction was most pronounced in the deep cervical plexus block group.
Nell’altro articolo invece viene ridimensionato l’effetto phrenic sparing del blocco del tronco superiore per la chirurgia della spalla:
Robles C, Berardone N, Orebaugh S Effect of superior trunk block on diaphragm function and respiratory parameters after shoulder surgery Regional Anesthesia & Pain Medicine Published Online First: 10 January 2022. Effect of superior trunk block on diaphragm function and respiratory parameters after shoulder surgery – PubMed (nih.gov)
Background The interscalene brachial plexus block has been used effectively for intraoperative and postoperative analgesia in patients undergoing shoulder surgery, but it is associated with high rates of diaphragmatic dysfunction. Performing the block more distally, at the level of the superior trunk, may reduce the incidence of phrenic nerve palsy. We hypothesized that superior trunk block would result in diaphragmatic paralysis rate of less than 20%.
Methods 30 patients undergoing arthroscopic shoulder surgery received superior trunk block under ultrasound guidance. Measurements of diaphragm excursion were determined with ultrasound prior to the block, 15 min after the block, and postoperatively in phase II of postanesthesia care unit, in conjunction with clinical parameters of respiratory function.
Results 10 patients (33.3%, 95% CI 17.3% to 52.8%) developed complete hemidiaphragmatic paralysis at the postoperative assessment. An additional eight patients (26.7%) developed paresis without paralysis. Of the 18 patients with diaphragm effects, seven (38.9%) reported dyspnea. 83.3% of patients with abnormal diaphragm motion (56.7% of the total sample) had audibly reduced breath sounds on auscultation. Oxygen saturation measurements did not correlate with diaphragm effect and were not significantly reduced by the postoperative assessment.
Conclusion Although injection of local anesthetic at the superior trunk level is associated with less diaphragmatic paralysis compared with traditional interscalene block, a significant portion of patients will continue to have ultrasonographic and clinical evidence of diaphragmatic weakness or paralysis.
Per concludere vogliamo segnalare questo articolo dal titolo fuorviante, dal quale sembrerebbe che non ci sia differenza fra anestesia generale ed anestesia neurassiale per I pazienti sottoposti a chirurgia protesica in percorsi fast track. In realtà l’articolo trae tale conclusione solo relativamente alle complicanze maggiori, ma fra i risultati rinforza notevolmente le importanti differenze che favoriscono l’anestesia loco regionale in termini di outcome.
Yap E, Wei J, Webb C, et Al Neuraxial and general anesthesia for outpatient total joint arthroplasty result in similarly low rates of major perioperative complications: a multicentered cohort study Reg Anesth Pain Med 2022 Jan 6;rapm-2021-103189. Neuraxial and general anesthesia for outpatient total joint arthroplasty result in similarly low rates of major perioperative complications: a multicentered cohort study – PubMed (nih.gov)
Background: Neuraxial anesthesia when compared with general anesthesia has shown to improve outcomes following lower extremity total joint arthroplasty. It is unclear whether these benefits are present in outpatient surgery given the selection of healthier patients.
Objective: To compare the effects of neuraxial versus general anesthesia on outcomes following ambulatory hip and knee arthroplasty.
Methods: Multicentered retrospective cohort study in ambulatory hip or knee arthroplasty patients between January 2017 and December 2019. Primary endpoint examined 30-day major postoperative complications (mortality, myocardial infarction, deep venous thromboembolism, pulmonary embolism, stroke, and acute renal failure).
Results Of 11 523 eligible patients identified, 10 003 received neuraxial anesthesia, while 1520 received general anesthesia. 30-day major complications did not differ between neuraxial anesthesia and general anesthesia groups (1.8% vs 2.3%; aOR=0.85, CI: 0.56 to 1.27, p=0.39). There was no difference in 30-day minor complications (surgical site infection, pneumonia, urinary tract infection; 3.3% vs 4.1%; aOR=0.83, CI: 0.62 to 1.14, p=0.23). The neuraxial group demonstrated reduced pain and analgesia requirements and had less postoperative nausea and vomiting (PONV). Median recovery room length of stay was shorter by 52 min in the general anesthesia group, but these patients were more likely to fail same day discharge (33% vs 23.4%; p<0.01).
Conclusion: Anesthesia type was not associated with an increased risk for complications. However, neuraxial anesthesia improved outcomes that predict readiness for discharge: patients had less pain, required less opioids, and had a lower incidence of PONV, thus improving the rate of same day discharge.
